Abstract
Background: Peripherally-inserted central catheters (PICCs) are commonly used during hospitalization for ease of access with blood draws and fluid and medication administration. PICC use is frequently complicated by catheter-related thrombosis (CRT). Current guidelines recommend 3-6 months of anticoagulation for patients with CRT after catheter removal. This recommendation is based on extrapolation of data on lower extremity thrombosis, as data is lacking regarding the efficacy and safety of more specific management strategies in upper extremity cases. Retrospective data exists to suggest catheter removal without anticoagulation is a sufficient and reasonable treatment option, particularly for patients at risk for bleeding; no prospective randomized data have been reported in this population. We aimed to examine the incidence of progressive thrombosis and bleeding in a retrospective cohort of patients with PICCs.
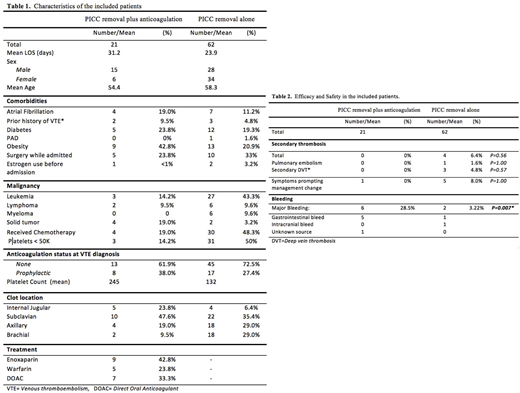
Methods: We performed a retrospective analysis of hospitalized adult patients diagnosed with CRT at our center from 2012 to 2018. We determined rates of progressive thrombosis and bleeding in cohorts of patients who underwent catheter removal vs. those who had catheters removed and received anticoagulation.
Results: Among 83 total patients, 62 were treated with PICC removal alone, while 21 underwent PICC removal and received therapeutic anticoagulation. Patients treated with PICC removal alone were more likely to have hematologic malignancy, receive chemotherapy, develop thrombocytopenia, and have brachial vein thrombosis. No patients in the PICC removal plus anticoagulation arm developed progressive thrombosis, while 6.4% of patients treated with catheter removal alone developed a secondary VTE event, including one PE, three DVTs; this difference did not reach statistical significance. Five patients (8%) treated with catheter removal alone also developed progressive symptoms leading to initiation of anticoagulation. Major bleeding was significantly more common in the PICC removal + anticoagulation arm (28.5% vs 4.8% p=0.007).
Conclusions: Catheter-removal alone results in significantly reduced major bleeding compared with catheter-removal plus anticoagulation. In select patients, catheter removal alone may be considered as an option for CRT, though larger, prospective trials are needed to clarify whether this practice is effective at reducing rates of progressive thrombosis.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.